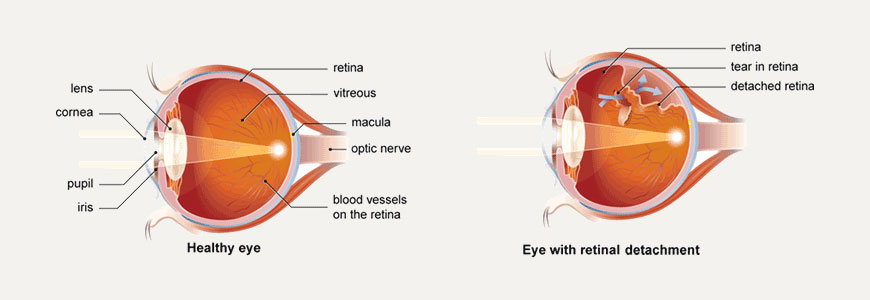
Retinal Detachment
Treating Retinal Detachment
If the retina has become detached and the detachment is too large for laser treatment or cryotherapy alone, surgery is necessary to "Re - Attach" the retina.
Without some type of retinal re - attachment surgery, vision will almost always be lost.
Scleral Buckling
The traditional surgery for Retinal Detachment is scleral buckling and is performed in the operation room under local or general anaesthesia. In this process, after cryotherapy is done to seal the retinal tears, a piece of silicone plastic is sewn onto the outside wall of the eye ( sclera ) over the site of the tear. This pushes ( buckles ) the sclera in toward the retinal tear and holds the retina against the sclera until scarring from the cryotherapy seals the tear.
This procedure is usually combined with placement of an encircling silicone band around the circumference of the eye to lessen the pulling of the vitreous on the retina. The surgeon may also drain fluid from underneath the retina and place a gas or air bubble into the vitreous cavity. These buckles and bands are left permanently and are not visible from outside. Success rates for re - attaching the retina with scleral buckling are approximately 90 - 95%.
Pneumo - Retinopexy
This is another type of surgery for re - attaching the retina. Instead of placing a buckle after cryotherapy, the surgeon injects a gas bubble inside the vitreous cavity of the eye. The patient is instructed to keep his or her head in a specific position so that the gas bubble seals the retina tear by its surface tension effect. Circulation of fluid through the tear stops and the retina is re-attached. The gas bubble in the eye expands for several days and takes 2 to 4 weeks to disappear. During this time air travel and travel to high altitudes must be avoided, because the gas may expand, thereby increasing the eye pressure, and cause damage to the optic nerve.
Vitrectomy
Occasionally, Retinal Detachment is so complicated and severe that it cannot be treated with either standard scleral buckling surgery or pneumatic retinopexy. Moreover scleral - buckling surgery fails approximately 5% to 10% of the time because excessive scar tissue grows on the surface of the retina. This scar tissue is very bad for the eye. It pulls on the retina, causing it to re - detach. Retinal re - detachment usually occurs four to eight weeks after the initial surgery. The vitreous pulls on the retina, detaching it from the back wall of the eye. The scar tissue also puckers the retina into stiff folds, like wrinkled aluminum foil. This condition is called proliferative vitreo - retinopathy ( PVR ). The only way to unfold and re - attach the retina is to cut away the vitreous and remove the scar tissue with vitrectomy surgery and then re-attach the retina. The surgeon uses a fibre - optic light to illuminate the inside of the eye and a variety of instruments ( scissors, forceps and laser probes ). The vitreous gel is removed as well as abnormal scar tissue, and replaced with fluid or air. Sometimes the natural lens or a previously existing intraocular lens ( IOL ) may have to be removed if the case is complicated. The holes and tears are sealed with laser, and fluid under the retina is drained. At times, vitrectomy is combined with placement of a scleral buckle. Often air, gas or silicone oil is placed in the vitreous cavity to hold the retina in place. If silicone oil has been used, it has to be removed at a later date as a separate surgical procedure.
Removing the vitreous and especially the scar tissue from the surface of the retina is a delicate process that requires the surgeon to lift and peel strands of scar tissue away from the retina. The surgery may take many hours in severe cases. SutureLess Vitrectomy is also available these days. If the retina is successfully re-attached, the eye will recover some sight, and blindness will have been prevented. However, the degree of vision that finally returns up to six months after successful surgery depends upon a number of factors. Unfortunately, success in re - attaching the retina ( anatomic success ) does not always translate into marked visual improvement ( functional success ). This is because of permanent damage to fine vision cells of the macula. In general, there is less visual return when the retina has been detached for a long duration, or there is a fibrous growth on the surface of the retina. It should be clearly understood that often the purpose of surgery for PVR is to give the patient an eye that would have some supporting vision and could serve as a "Spare Tyre", if the other eye ever loses vision entirely.
Vitreous Surgery for Primary Retinal Detachment
Vitreous surgery is now often undertaken for primary detachments when the tears are very large or placed very far back ( posteriorly ) on the retina, when there is a macular hole causing detachment, or if there is blood in the vitreous blocking a clear view of the retina. Success rates for these cases are much better with vitrectomy than with scleral buckling alone.
What are the complications of surgery ?
Even though the surgery for Retinal Detachment is generally successful, certain complications can occur. They include drooping of the upper lid and double vision, which are temporary. Serious complications include infection, bleeding severe enough to interfere with vision, glaucoma and cataract formation. However, these complications are very infrequent. Retinal re - detachment is the most commonly occurring problem. If this occurs, your surgeon will discuss the chance that a re-operation will successfully re - attach the retina. It is important for the patient to know that surgery may fail due to complications, or simply due to the progressive nature of the retinal disease.
What are the complications of surgery ?
Even though the surgery for Retinal Detachment is generally successful, certain complications can occur. They include drooping of the upper lid and double vision, which are temporary. Serious complications include infection, bleeding severe enough to interfere with vision, glaucoma and cataract formation. However, these complications are very infrequent. Retinal re - detachment is the most commonly occurring problem. If this occurs, your surgeon will discuss the chance that a re - operation will successfully re - attach the retina. It is important for the patient to know that surgery may fail due to complications, or simply due to the progressive nature of the retinal disease.
What may I do after surgery ?
You must stay at home for at least three weeks, traveling should be avoided except to visit the doctor. After surgery you will be given written instructions regarding medication and precautions to be taken. You should carefully observe these instructions. You may be advised to lie on your side or stomach while sleeping or resting.
What are the chances of success ?
In most cases (85%) the retina can be reattached with a single operation. Occasionally additional surgery is necessary; this brings the final cure rate up to approximately 95%. The final degree of clarity of vision will not be known for three months. If you had lost your reading vision before surgery, you should find considerable improvement but probably not 100%. If your reading vision was not lost before surgery, good vision will be retained ( after convalescence ) in more than 90% cases. In 5% cases the retina may not re - attach, necessitating further surgery.
What are the common side effects and complications of the surgery ?
Your vision will be blurred. The eye will be painful, red and swollen and there may be some mucus discharge. The pupil will be large and you may see double. These side effects are usually temporary and last only a few weeks. In many cases the eye will become more near - sighted this can be corrected with spectacles. Over 90% cases have no significant complications. Occasional problems include bleeding or infection or re - detachment. Very rarely such complications could lead to the loss of all vision. Anaesthesia related complications are also rare the anaesthetist will discuss these with you.
What about the future of my retina ?
If the retina remains attached for three months after surgery, the chance of recurrence is only 10%. If the retina of your other eye appears normal at this time, the chance of developing a detachment later on is approximately 12% in the eye that has not been operated.
Can retinal detachment be prevented ?
In some cases the retina is more fragile and prone to formation of holes or breaks. If these are detected and sealed in the early stages by laser or cryosurgery, Retinal Detachment can be prevented. People who are likely to develop Retinal Detachment should have periodic examinations done after dilation of the pupils. Some of the situations where this is desirable are :
History of Detachment in One Eye
Family History of Retinal Detachment
History of Injury to the Eye or Its Surrounding Bones
History of Flashes and Floaters
Sudden Onset of Floaters or Change in the Character of Floaters