Diabetic Retinopathy
What is diabetic retinopathy ?
Diabetes damages blood vessels in the rear of the eye. This condition is called Diabetic Retinopathy. It can lead to vision loss or blindness. You already may have Diabetic Retinopathy, of be at risk for it. But you can take steps to reduce your risk of vision.
Diabetes and Vision Loss : A glance out window helps you choose between a sweater and a raincoat. Reading to your grandchild turns a normal day into something special. Having diabetes may threaten your visual link with the world. That's frightening. But you can work with your healthcare team to manage your diabetes and keep Diabetic Retinopathy under control.
Diabetic Retinopathy and its Symptoms : At first, Diabetic Retinopathy may cause no vision loss or other symptoms. But over time, it can still harm vision. If you have symptoms of Diabetic Retinopathy, the may include - Having blurry, darkened or cloudy vision. Seeing floaters ( dark spots ) or black lines.
Learning about Diabetic Retinopathy : Your healthcare team will help you learn more about Diabetic Retinopathy and how to control it. When you meet with your doctor, ask questions. Take notes, or have a family member or friend take notes. And read this booklet to learn more.
Your Ophthalmologist : Ophthalmologists are medical doctors. They oversee vision care, diagnose and treat eye disorders, and perform surgery on the eye. Together, you and your ophthalmologist will design a treatment plan to protect your vision. Keeping your appointments and following your treatment plan will help save your sight.
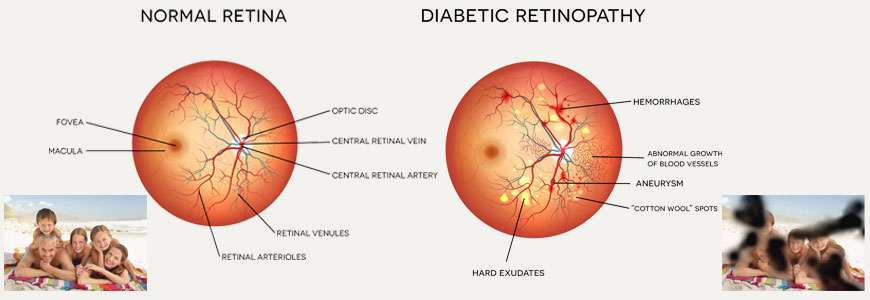
Eye Anatomy
The eye receives and processes light. The retina ( the inside lining of the eye ) turns light into nerve signals. These become visual images in the brain. Tiny capillaries ( Blood vessels ) bring blood nourish the retina.
How You See : Light enters the eye through pupil. The light passes through the clear tissue of the lens and the vitreous ( the clear gel that fills the eye ). The light then strikes the retina, where special cells send signals to the brain. The brain turns these signals into visual images what you see.
The Healthy Retina
A Healthy Retina Includes :
The Macula, the area of the Retina where Sharp Central Vision takes Place
The Fovea, the most Sensitive part often Macula
The Periphery, Which Surrounds the Macula
This Provides Periphery (side) Vision what we see Outside our Sharp Central Vision
Capillaries that Nourish the Retina with Blood
Diabetes and The Eye
Diabetes can cause capillaries on the retina to leak or collapse. Then fragile new capillaries may grow on the retina, causing more damage. Both types of damage to the retina are forms of Diabetic Retinopathy.
An Unhealthy Retina : Damaged capillaries can interfere with vision. They can also reduce the amount of blood nourishing the retina. Reduced blood flow causes fragile new capillaries to grow in the retina ( neaovascularization ). As Diabetic Retinopathy progresses, vision loss can get worse.
Damages from Existing Capillaries : Existing capillaries may - Form microaneurysms ( bulges in the capillaries wall ), These may leak fluid and fatty substances ( hard exudates ), This leakage can cause macular edema ( swelling ), Close up, forming cotton wool spots( soft exudates ), Cause bleeding on the retina ( dot - blot hemorrhages ).
Damages from New Capillaries : Fragile new capillaries may - Bleed into vitreous, Cause the vitreous to pull on the retina ( traction ). Traction cam cause bleeding, creates scar tissue, or dislodges the retina from the back of the eye ( Tractional Retinal Detachment ).
How your Vision can Changes
Diabetic Retinopathy may progress from its early stage ( non proliferative ) to its later stage ( proliferative ). Either stage may cause vision loss. There may be little or no vision loss at first. But even without early vision loss, Diabetic Retinopathy still damages the retina. Severe vision loss even blindness may occur later.
Non Proliferative Diabetic Retinopathy : At this stage, capillaries in the retina have been damages. But there's no growth of fragile new capillaries on the retina. This stage of Diabetic Retinopathy may cause no symptoms or it may result in some vision loss. This stage is also called background Diabetic Retinopathy.
Proliferative Diabetic Retinopathy : At this stage, fragile new capillaries begin to grow on the retina. This capillary growth may result in bleeding or traction, causing severe vision loss. This stage is common in people who have Diabetic Retinopathy for a long time.
Managing your Health
You can greatly reduce risk of vision loss from Diabetic Retinopathy by managing your overall health and take care of other health problems that can make Diabetic Retinopathy worse.
Manage your Diabetes : The best way to protect your vision is to keep your blood sugar level in healthy range. Check your blood sugar regularly. Follow your diabetes management plan and work with your primary care physician or endocrinologist if you are having trouble in keeping your blood sugar in healthy range.
Control your Risk Factors : Other factors that damage blood vessels can make Diabetic Retinopathy worse. These include - High Blood Pressure, Smoking, High Cholesterol, Work with healthcare team to control these problems and help lower your risk. A diabetes educator can help you control blood pressure and high cholesterol. He or she can also recommend stop smoking programmes.
Evaluation of your Eyes
You need to visit your ophthalmologist for a complete dilated eye examination at least once yearly ( more often if you are pregnant ). During the examination, he or she will review your medical history, check your vision, and examine your eyes.
Your Medical History : Your ophthalmologist will ask about - Your diabetes type, history, treatment ( such as insulin ) and how you monitor your blood sugar level, Your family's health, including whether any relative has had Diabetes or Diabetic Retinopathy, Any disease, surgeries or other medical procedures you have had, Any medications, herbs or supplements you use, including those you buy over the counter.
Your Eye Examination : Your ophthalmologist uses an eye chart and other special tools to check your vision. Them he or she will examine your eyes for signs of disease. After eye drops dilate ( widen ) your pupils, you may have one or more of the following tests :
Tonometry
Slit Lamp Examination
Ultrasound this uses sound waves to create an image of your eye. If may be used if there is blood in the vitreous.
Fluorescein Angiography
Fluorescein angiography uses special photographs of the retina to reveal changes in the capillaries. Before this procedure, dye is injected into your arm or hand. The dye highlights capillaries in the retina. Photographs are taken before and after the dye in injected. During the procedure, you may briefly feel some nausea, after the procedure, your skin, eye, and urine may appear yellow for a few hours.

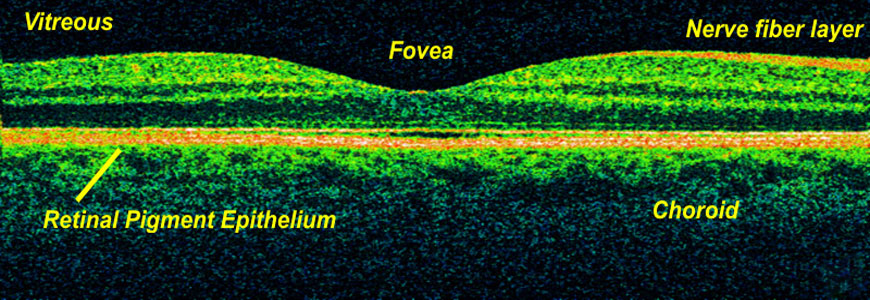
Optical Coherence Tomography
Optical Coherence Tomography (OCT) is a non - invasive imaging test that uses light waves to take cross - section pictures of your retina, the light - sensitive tissue lining the back of the eye.
What's the next step ?
Your ophthalmologist will work with you to design a treatment plan that is best for you. You may need more than one of the treatment - Laser photocoagulation, to control leaking capillaries and prevent growth of new capillaries, Intravitreal injections of Anti VEGF drugs eg Avastin, Lucentis, Vitrectomy, to remove a cloudy vitreous and scar tissue, Other surgery or medications as recommended by your ophthalmologist
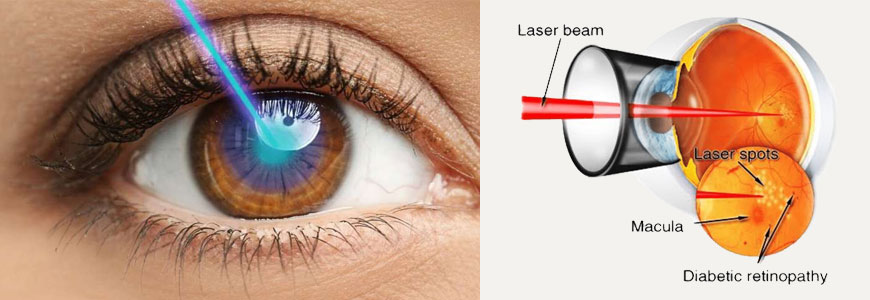
Having Laser Treatment
Laser photocoagulation uses a laser ( a high energy light source ) to treat Diabetic Retinopathy. This treatment doesn't cure Diabetic Retinopathy. But it may slow or halt the progress of the disease.
How is the laser used ?
During the procedure, a laser beam is focused on the retina. The laser seals weak capillaries. It also slows or stops new capillary growth.
Types of Laser Treatment : The type of treatment you receive depends on the extent and location of damaged capillaries. Treatment may take from afew minutes to half hour or so,. You may need more than one treatment session or type of treatment.
Preparing for Laser Treatment : Tell your ophthalmologist about all medications, herbal remedies, or supplements you use, such as aspirin, ibuprofen or blood thinners. Arrange for someone to drive you home after surgery.
During Laser Treatment : Laser treatment would be done at the hospital. You will be awake during treatment. The doctor uses eye drops to dilate your pupil. The doctor may require to hold a special contact lens against your eye.
Controlling Pain : Laser treatment may cause some discomfort. If so you will be given medication to control it. If the discomfort continues, tell your doctor.
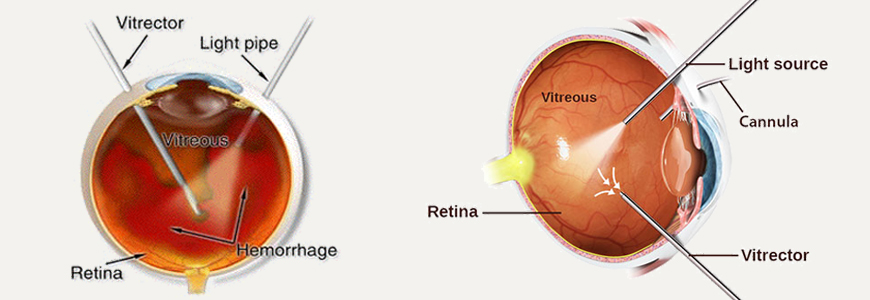
Having Vitrectomy
If blood or debris in the vitreous is clouding your vision, your doctor may recommend Vitrectomy. This surgery removes the cloudy vitreous. This vitreous is replaced with fluidor gas. If vision problems continue after Vitrectomy, you may need additional surgery.
Preparing for Vitrectomy : Before your surgery, tell your doctor about medications, herbal remedies, or supplements you use. These may include aspirin, ibuprofen, blood thinners etc. before surgery, you will meet with an anaesthesiologist ( a doctor who provide medications to control pain ).
During Vitrectomy : Tiny instruments are inserted through small incisions in the sclera. The vitreous is removed. It is replaced with ringer lactate solution, a gas or silicone oil to hold the retina in place. Surgery may take several hours.
After Vitrectomy : You would require admission at the hospital for particular time period. You will be told how to care for your patch or bandage. Do not rub or touch your eye. You will receive medications to control pain.
Working with your Healthcare Team
You are the most important member of your healthcare team. Work with your doctor and other healthcare providers to manage your diabetes. Keep visiting your ophthalmologist for regular eye examinations and vision care.
When Schedule an Eye Examination : People with diabetes should examinations at least once a year. More frequent medical eye examinations may be necessary after diagnosis of Diabetic Retinopathy. Pregnant women with diabetes should schedule an appointment in first trimester because retinopathy can progress quickly during pregnancy. Pregnant women with diabetes should schedule an appointment in the first trimester because retinopathy can progress quickly during pregnancy. If you need to be examined for glasses, it is important that your blood sugar be in consistent control for several days when you see your ophthalmologist. Rapid changes in blood sugar can cause fluctuating vision in both eyes even if retinopathy is not present. Youshould have eyes checked promptly if you have visual changes that - Affect only one eye, Last more than a few days, Are not associated with changes in blood sugar When you are first diagnosed with diabetes you should have your eye checked, Within five years of diagnosis if you are 30 years old or younger, Within few months of the diagnosis if you are older than 30 years.
Follow your Treatment Plan : Your treatment plan will help your reduce your risk of vision loss. To control diabetic retinopathy - Check your blood sugar as directed, Take care of your overall health. Don't smoke. Follow your doctor advice about exercise and diet, Report vision changes or other symptoms to your ophthalmologist right away.